Diabetic Retinopathy: What you really need to know about your eyes and diabetes
When it comes to diabetes, people often talk about the heart and kidneys, but the eyes get left out

Most conversations about diabetes stay focused on sugar levels, food choices, and long-term health, but the eyes rarely enter the discussion. It surprises many people to learn that the condition can quietly affect the retina, the part of the eye that handles sharp vision.
Asst Prof Dr Wijak Kongwattananon, an ophthalmologist at MedPark Hospital Bangkok, often meets patients who are hearing about diabetic eye disease, including diabetic retinopathy, for the first time. He explains, “diabetes, fundamentally it’s a disease of high blood sugar. And over time, that excess sugar damages the small blood vessels throughout the body and the eye, and specifically the retina.”
The retina plays a vital role in how we see the world. Yet it is also delicate, and the blood vessels that feed it respond quickly to changes in blood sugar. This is why it’s important for us to be aware of diabetic retinopathy.
On this page
| Click to jump to section | Summary |
|---|---|
| How diabetes affects the retina | High blood sugar damages the tiny blood vessels in the retina, causing leakage, swelling, poor oxygen supply, and abnormal vessel growth that can lead to vision loss. |
| Does it take years of struggling with diabetes before this problem starts? | Diabetic retinopathy can develop early, especially when blood sugar control is poor or when Type 2 diabetes has gone undiagnosed for years. |
| How common is diabetic retinopathy? | About one in four people with Type 2 diabetes have some form of diabetic retinopathy, often without any noticeable symptoms. |
| How is diabetic retinopathy diagnosed? | The condition is detected through dilated eye exams, retinal imaging, fundus photography, and OCT scans that reveal early retinal changes. |
| What doctors look for during the eye exam | Specialists check for microaneurysms, small haemorrhages, fluid leakage, and fatty deposits that signal retinal damage. |
| Technology and AI have become advanced, but doctors remain essential | Digital imaging and AI help identify and track retinal changes, but specialist interpretation and patient discussion remain crucial. |
| What treatment options are available for diabetic retinopathy? | Treatments include eye injections, laser therapy, and surgery in severe cases, with early treatment offering strong protection for vision. |
| Is it scary? | While injections can sound intimidating, procedures are quick, well explained, and generally cause minimal discomfort for patients. |
| How can you protect your eyes if you have diabetic retinopathy? | Long-term protection depends on good blood sugar control, managing blood pressure and cholesterol, avoiding smoking, and having yearly eye exams. |
How diabetes affects the retina

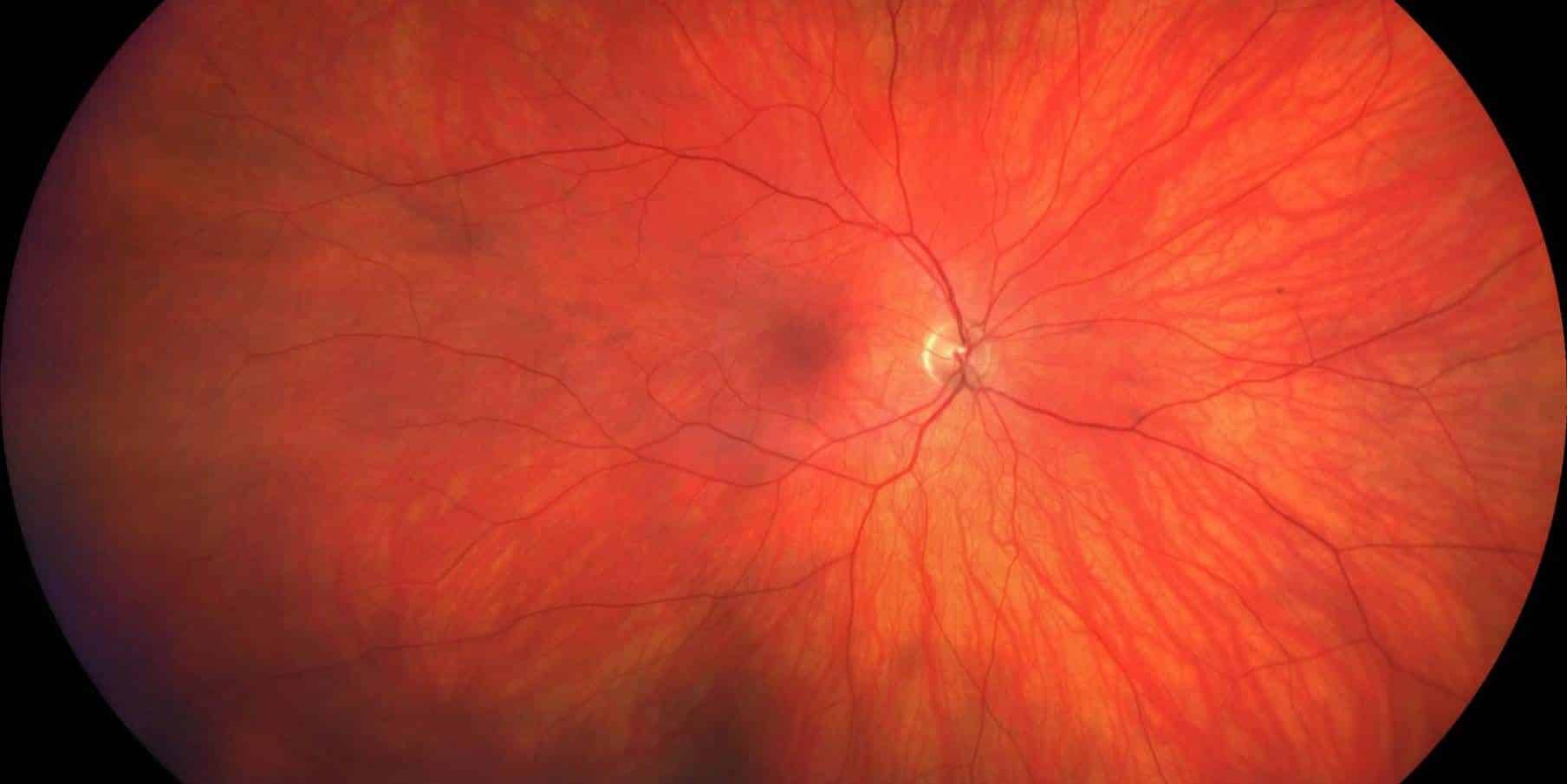
The retina is a thin, delicate layer at the back of the eye. “The retina is like the film in a camera,” Dr Wijak describes. It captures light and sends signals to the brain, allowing you to see clearly. Because it is full of tiny blood vessels, it is especially vulnerable to damage from high blood sugar.
When blood sugar stays high for long periods, the vessel walls weaken. “They can swell, causing them to leak fluid and blood,” he explains. The central part of the retina, called the macula, is especially sensitive. When fluid collects there, it becomes diabetic macular oedema, a very common cause of vision problems in people with diabetes.
If the disease progresses, the retina struggles with oxygen. “The retina is starved of oxygen, and tries to grow new abnormal and very fragile blood vessels,” he says. These vessels bleed easily and form scar tissue that can pull on the retina. “This can lead to severe vision loss or even retinal detachment.”
What makes this more complicated is that the early stages feel like nothing at all. Many patients still see perfectly.
Does it take years of struggling with diabetes before this problem starts?

People often believe diabetic retinopathy only appears after a long time. According to Dr Wijak, that isn’t always the case.“It is a misconception that it only appears after many years. It can certainly appear earlier, particularly if sugar control has been poor.”
This is especially true for Type 2 diabetes. Some people have had high blood sugar for years without knowing it. By the time they receive a diagnosis, subtle retinal changes may have already developed. Because of this, Dr Wijak recommends screening right away. “Screening should be done immediately upon diagnosis. Many patients may have had the condition for years before it was officially discovered.”
How common is diabetic retinopathy?
The condition is more common than most people think. “Around one in four, or twenty-five percent, of people with Type 2 diabetes have some form of diabetic retinopathy,” Dr Wijak says.
And most have no idea anything is wrong. “Usually the patient has no symptoms when they come to see us.” Vision can be crystal clear even when damage has already begun.
How is diabetic retinopathy diagnosed?

If you’ve never had a diabetic eye screening, you might imagine something complicated or uncomfortable. In reality, the process is easy and straightforward.
At MedPark, the exam starts with a vision check and eye pressure measurement. Then dilating drops are used to open the pupil. This allows the doctor to see the back of the eye clearly. As Dr Wijak explains, dilation “opens up the window to the back of the eye, allowing the doctor to get a clear, wide field of the entire retina.”
Advanced tools like fundus photography and OCT (Optical Coherence Tomography) help take detailed images. “These tools help detect early signs on the patient’s retina,” he says. OCT scans show cross-sectional images of the retina at a microscopic level, revealing swelling long before symptoms appear.
The whole process typically takes one to two hours. “Patients only see me once a year, and they spend around two hours to make sure that they are still okay,” he says.
What doctors look for during the eye exam
Retinal specialists look for tiny but telling changes. “Microaneurysms, tiny haemorrhages and signs of leaking, which appear as yellow fatty deposits called hard exudates,” Dr Wijak explains.
Finding these signs early allows treatment to begin before vision is affected.
Technology and AI have become advanced, but doctors remain essential
Digital retinal photography and OCT imaging allow specialists to detect small changes with precision. These tools also make it easy to track progress year by year. According to Dr Wijak, “We can detect even subtle progression.”
Artificial intelligence is also helping in areas with fewer specialists. “AI can analyse a digital retinal photograph and determine if a patient has signs of diabetic retinopathy,” he says. This improves access to early screening, especially in community hospitals.
This is a huge help in areas with fewer specialists. However, patients at MedPark still see a real retinal specialist because conversations, reassurance, and explanations remain essential.
What treatment options are available for diabetic retinopathy?
Hearing that you may need treatment for your eyes can feel overwhelming, especially if this is your first time visiting a retinal specialist. But modern treatment is far gentler than most people expect.
For many patients, the first-line treatment is an injection of anti-VEGF medication or steroids. This reduces swelling and stops abnormal vessel growth. According to Dr Wijak, “the procedure is quick and nearly painless.” The doctor will numb the eye completely beforehand. Most patients feel only slight pressure. “The injection itself takes just a few seconds,” he says.
Laser treatment is another option. It targets areas of the retina that lack oxygen, helping stabilise the disease. In severe cases involving large bleeds or retinal detachment, patients may need surgery. But early treatment is highly effective. “Anti-VEGF injections can stabilise vision or even improve vision in over ninety percent of patients.”
Is it scary?
Many people are understandably nervous when they hear the word “injection.” Dr Wijak sees this every week. “Everyone who hears they are going to be injected reacts the same way,” he says. He takes time to explain every step, and sometimes patients ask to hold his hand. “It’s totally fine,” he says with a smile.
Some patients feel calmer when they see their own retinal images. Dr Wijak uses the photos to show exactly what’s happening and what needs to be controlled. “If I share their image, they understand their own eye better,” he says.
How can you protect your eyes if you have diabetic retinopathy?

While treatment can repair damage, long-term protection comes from everyday health choices.
Blood sugar management remains the most important factor. “Strict control can significantly delay or reduce the risk of eye complications.” Blood pressure also plays a major role because high pressure puts stress on those delicate retinal vessels.
Cholesterol and smoking influence the condition as well. “Smoking severely thickens blood flow and oxygen, so it makes retinopathy worse.”
“Your eye is precious, and most diabetes-related vision loss is preventable. So please get your eyes checked every year. With today’s technology and treatments, I’m confident that we can protect your vision for life,” Dr Wijak advises.
A yearly eye exam may feel easy to put off, but it is one of the simplest ways to protect your sight for the long term. To get screened or treated for diabetic retinopathy, you can schedule an appointment with the specialists at MedPark Hospital.
Sponsored
Latest Thailand News
Follow The Thaiger on Google News: