JN.1 Covid-19 variant detected in Thailand: 40 cases and counting
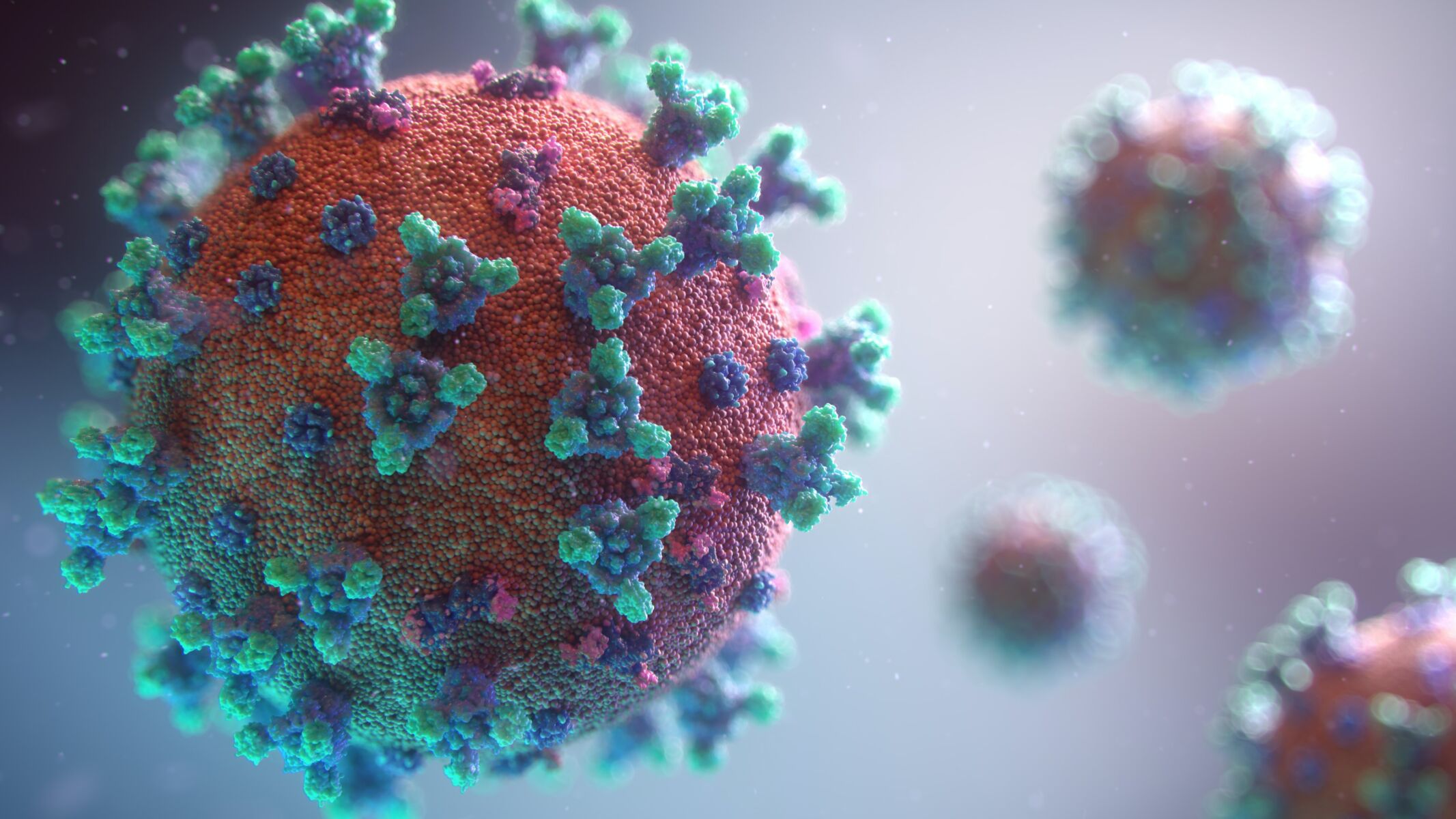
The Covid-19 variant JN.1* has been detected in Thailand, with 40 cases reported so far. Thai health officials are closely monitoring the situation as it is speculated to replace the XBB variant as the dominant strain. The JN.1 strain was first detected in Thailand in October last year and increased significantly in December last year.
Yongyot Thammavut, Director of the Department of Medical Sciences, Ministry of Public Health, revealed that since early 2023, the XBB.1.16* hybrid strain had been the dominant strain in Thailand until September. However, it began to decline, and the XBB.1.9.2* variant started to replace it. Recent genome sequencing results of the Covid virus in the lab from November last year to January 15 this year, showed a decrease in the XBB.1.9.2* hybrid strain, while the proportion of JN.1* significantly increased.
“From current data, JN.1* infections have been found in Health Areas 2, 4, 5, 6, 7, 11, 12, and 13, with general respiratory symptoms such as fever, cough, and phlegm. No deaths from the JN.1* infection have been reported yet. Currently, there are 40 JN.1* infections in Thailand, and there are no two mutation types yet”
Yongyot also stated that the department and lab network have been monitoring the situation of SARS-CoV-2 variants in Thailand since early 2022. They found Omicron variants BA.1, BA.2, BA.4, BA.5 and other sub-varieties in the lineage. Currently, the Omicron variant is the main strain spreading in the country.
The World Health Organisation (WHO) continues to prioritise monitoring ten Omicron sub-variants due to their increasing prevalence or advantage in the rate of increase compared to other strains and mutations concerning the advantage in disease causation, namely:
Variants of Interest (VOI) – five strains: XBB.1.5*, XBB.1.16*, EG.5*, BA.2.86*, and JN.1*.
Variants under monitoring (VUM) – five strains: DV.7*, XBB*, XBB.1.9.1*, XBB.1.9.2*, and XBB.2.3*.
Sub-variants
On December 18, last year, the WHO designated the JN.1* variant as a VOI. The JN.1* variant is a sub-variant of BA.2.86* that has a mutation on the spike different from BA.2.86, namely L455S (the amino acid at position 455 changes from Leucine to Serine), significantly increasing its ability to evade immunity. JN.1* has a growth advantage over XBB.1.9.2* up to 73%, reported Sanook.
In early this year, there were reports of additional mutations of JN.1* at position F456L (Phenylalanine replaced by Leucine at position 456), combined mutations at two positions L455S and F456L, called Slip mutation. The first cases of JN.1* with two mutations were reported in France, now found worldwide with 41 cases (as of January 15 this year).
Yongyot stated that the global VOI situation from the GISAID central database for week 48 (October 27 – December 3, last year) found the most EG.5* in proportion, 36.3%, followed by JN.1* found in a proportion of 27.1%. EG.5* has a gradually decreasing rate of detection, while JN.1*, which has a growth advantage and evasion characteristics, has a continuously increasing detection rate in the past 28 days.
The most common VUM strains were XBB.1.9.1* in a proportion of 3.3% and DV.7*, a strain with a Flip mutation, and two adjacent mutations, namely L455F and F456L. These mutations aid attachment to human cell surfaces and evade immunity effectively. However, the proportion of DV.7* is continually decreasing, and currently, no reports increase the severity of the disease.
“The department and lab network continuously monitor the change in strains by collecting positive samples of the COVID virus from ATK or real-time RT-PCR testing from all over the country. They sequence the entire genome and publish it regularly through the global GISAID database. Monitoring current strains prevalent in the country can help enhance lab readiness to handle future outbreaks,” Yongyot stated.
Prevention measures according to public health standards still apply to all strains. Symptoms and severity, depend more on the immune system and overall health of the individual than the type of infecting strain.
Latest Thailand News
Follow The Thaiger on Google News: